Lp(a)
Primary care physicians don't usually check lipoprotein (a), but we should. Elevated levels (≥50 mg/dL) are a genetic condition (LPA gene) that affects about 20% of people and significantly increases atherosclerotic coronary vascular disease and aortic valve stenosis.
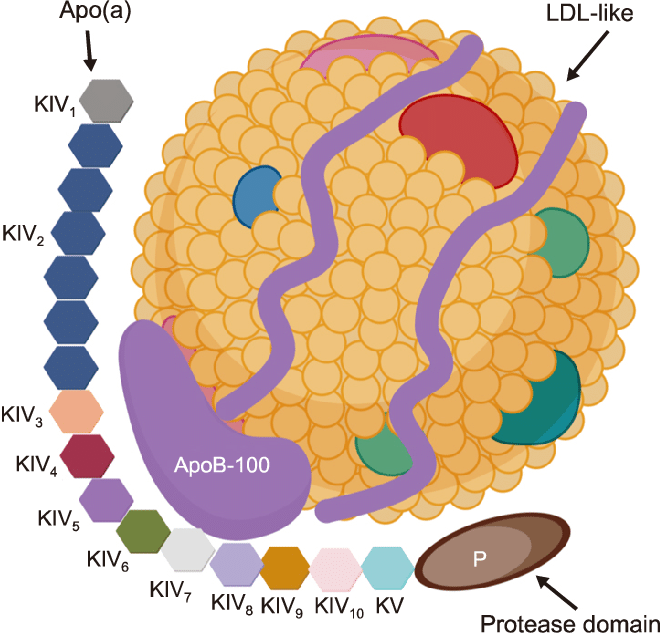
Primary care physicians don't usually check lipoprotein (a), but we should. Elevated levels (≥50 mg/dL) are a genetic condition (LPA gene) that affects about 20% of people and significantly increases atherosclerotic coronary vascular disease and aortic valve stenosis.
Lp(a) does not change in adults over time (except for increases during inflammatory states), so it typically needs to be checked only once in a lifetime in a healthy person, perhaps at their first lipid screening.
Lp(a) Treatments Today
Diet, exercise, and statin drugs do not reduce Lp(a) levels. These usual treatment options that reduce LDL but do not have a helpful effect on Lp(a) might be the reason for typically not checking Lp(a) in the past.
PCSK9 inhibitors reduce Lp(a) by 26%, and in the FOURIER trial, as noted by UpToDate:
evolocumab reduced the risk of coronary heart disease death, myocardial infarction, or urgent coronary revascularization. After adjustment for change in LDL-C, each 25 nmol/L reduction in Lp(a) from evolocumab led to a 15 percent relative risk reduction (95% CI 2.0-26.0 percent). Evolocumab reduced the risk of coronary heart disease death, myocardial infarction, or urgent revascularization by 23 percent in patients with a baseline Lp(a) >median (37 nmol/L; hazard ratio 0.77, 95% CI 0.67-0.88) and in those with a baseline Lp(a) ≤median by 7 percent (hazard ratio 0.93, 95% CI 0.80-1.08; p interaction = 0.07).
Apheresis is also used to treat high Lp(a). While effective for lowering Lp(a) by as much as 75%, it is expensive and inconvenient, and randomized clinical trials prove that reduced cardiovascular event rates are lacking.
New Lp(a) Therapies Tomorrow
"Antisense oligonucleotides (ASO) shows good safety and strong efficacy with up to 90% reductions. The ongoing CV outcomes study Lp(a)HORIZON will provide a first answer as to whether selective Lp(a) lowering with ASO reduces the risk of major CV events." (Rhainds, et al.)
The Lp(a)HORIZON trial is detailed at https://clinicaltrials.gov/study/NCT04023552. This randomized, placebo-controlled trial sponsored by Novartis uses a monthly injection of an experimental antisense oligonucleotide (pelacarsen; TQJ230) vs. placebo. The 8,323 participants have Lp(a)>=70 and established cardiovascular disease. If it shows a significant reduction in cardiovascular events, it may become a standard of care for those with elevated Lp(a) and whatever additional criteria the FDA specifies based on the clinical trial evaluation.
Clinical trials using siRNA approaches to lower Lp(a) were successful. Further trials are ongoing to see if siRNA approaches also lower cardiovascular events in those with high Lp(a).
Lp(a) Screening - For Everyone?
Screening will become more common now that effective treatments are being developed to lower elevated Lp(a) - and, we hope, lower major cardiovascular events that the current clinical trials are determining.
The 2023 recommendations from the American College of Cardiology are:
- Lipoprotein(a) (Lp[a]) is an independent risk factor for atherosclerotic cardiovascular disease (CVD) and calcific valvular aortic stenosis.
- Lp(a) exhibits significant race/ethnic variations, with levels highest among persons of African ancestry.
- Lp(a) levels typically do not change after 5 years of age except during times of significant inflammation, liver disease, or kidney disease; hence, levels should be interpreted cautiously during these times.
- Current guidelines support once-in-a-lifetime measurement in most individuals with increased risk of atherosclerotic CVD.
NIH recommends:
In the U.S., Lp(a) testing is recommended for people younger than age 65 who have had a heart attack, those with a family history of premature heart disease, and those with elevated LDL cholesterol who haven’t responded to statins, cholesterol-lowering drugs that can lower LDL levels by about 30%.
Since elevated Lp(a) levels are largely due to genetic risks and don’t fluctuate much in response to modifiable risks, such as exercise, a one-time screening would be sufficient for most people, the experts noted. In Europe and Canada, Lp(a) screenings are recommended for everyone.
The argument for testing everyone at least once for Lp(a) was published in June 2024 in the European Heart Journal:
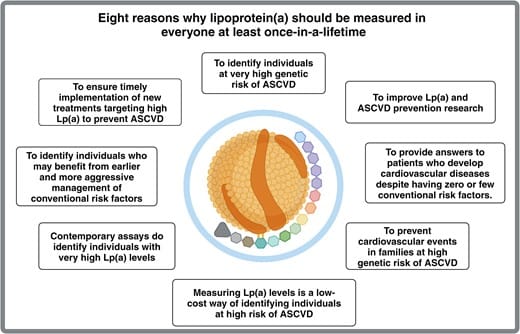
Cleveland Clinic also argues for broader Lp(a) testing:
“We want clinicians to start assessing Lp(a) now so that when Lp(a)-targeted therapies become available, we’ll be ready to treat the patients who need them,” Dr. Nissen concludes.
What does an Lp(a) test cost? This varies according to the lab used, but the current price is $55 if ordered through walkinlab.com, where one can order self-pay labs without your doctor needing to order them. The price might be much lower if the volume was large from everyone getting routine screening one time.