Salt Sensitivity
The Yanomano tribe has a low salt intake (perhaps <100 mg/day) and a high potassium intake from fruits and vegetables. Blood pressure does not rise with aging!

We are often told to avoid salt (sodium chloride) and keep it to 1,500 mg daily to protect our heart and blood pressure! But we hear others say don't worry about it; if we are healthy, our kidneys compensate and excrete excess salt. What is the best primary care advice about salt intake?
Some people are salt-sensitive, so salt restriction is essential for their health. Others are not. Their kidneys excrete excess salt, and restricting salt is not crucial for blood pressure control. However, salt resistance has limitations, especially as we age. Modern societies have a massive salt intake compared to some primitive societies.
There are also different salts. To a chemist, sodium chloride and potassium chloride are both salts. Table salt with sodium is the culprit for blood pressure and cardiovascular concerns. "Salt substitutes" we can buy in the grocery store are often potassium chloride. Using these has been shown to reduce strokes and blood pressure by up to 24% in some groups.
Let's review:
- Yanomamo tribe's no-sodium diet
- England's population experiment with restricting salt (NaCl) in processed foods
- Population advice vs. individual advice
- American Heart Association guidelines
- Blood pressure and salt (sodium and potassium salts)
- Kidney processing of salt and blood pressure
- Who is salt-resistant?
- Which salt is best?
Yanomamo tribe's no-sodium diet
Mancilha-Carvalho & Souza e Silva reported on the results of the INTERSALT study. The study included 10,079 people aged 20-59 from 52 populations in 32 countries. Each center enrolled 200 people, 25 in each age group. They reported:
The data analysis of 4 isolated populations (Yanomami Indians, Indians from Xingu, rural population of Kenya, and rural population of Papua, New Guinea) showed that neither blood pressure elevation with age is inevitable, nor is the high prevalence of hypertension. With a urinary sodium excretion ranging from 0.9 mmol/day to 51 mmol/day (compared with the mean of 165 mmol/day in the other 48 centers), blood pressure means were clearly lower in those 4 centers than in the remaining 48, blood pressure elevation with age was minimum or even negative, and hypertension virtually did not exist.
The mean blood pressure for the Yanomani tribe was the lowest of all centers: 95/61 mm Hg. The percentage of hypertensive individuals was 0%. 24-hour urine sodium excretion was <1 (mmol-median). The median BMI was 21.2. There was no alcohol ingestion.
Oliver et al. also studied the tribe and reported:
The Yanomamo are seldom obese and rarely demonstrate weight gain with advance in age. Furthermore, they are physically a highly active people with an overtly aggressive life style very different from that of present western culture. A role for other factors [than sodium] in these findings regarding blood pressure cannot be excluded.
This blog is available as an audio podcast on Spotify: https://podcasters.spotify.com/pod/show/joe-breault-md-scd/episodes/Salt-Sensitivity-e2kae77
England's population experiment with restricting salt (NaCl) in processed foods
As reported in The Guardian:
Salt is a significant cause of high blood pressure, which leads to tens of thousand of people a year suffering or dying from a heart attack or stroke.
The average amount of salt that people in England consumed fell by almost 20% after the Food Standards Agency (FSA) initiated a programme in 2006 in which food manufacturers reduced the salt content of scores of different types of processed and prepared foods.
Due to political reasons, the government abandoned forced limits on salt in processed foods in 2011, instead just giving salt recommendations to processed food manufacturers, and as a result, the same article reported:
After the change average intake rose again, from 7.58g a day in 2014 to 8.39g a day in 2018, according to the study, which has been published in the Journal of Hypertension. It has “stalled” since, the authors found from their analysis of published health figures.
A team of researchers led by Dr Jing Song from Queen Mary University of London (QMUL) calculated that if the salt reduction drive had continued, average intake would have fallen by a further 1.45g a day between 2014 and 2018. “This would have prevented over 38,000 deaths from strokes and heart disease in just a four-year period, of which 24,000 would have been premature,” they said.
Many studies have analyzed England's experiment. My conclusions from reviewing the England data are:
- Governments forcing the food industry to reduce salt in processed foods is good for population health (fewer heart attacks and strokes) and for saving money (fewer costs to the health care system).
- Reducing salt in processed foods is probably bad for the food industry. It reduces their profits since it makes processed foods less addictive, and they probably sell less of them.
- We already know processed foods are bad for us, and we should minimize or avoid them in a healthy diet. Since the average person's salt intake is primarily from processed foods, a healthy diet that avoids processed foods is already relatively low in salt.
- England's health improvements were achieved by reducing its salt intake from 9.5 grams a day to 7.5 grams a day. Europe typically reports salt use as NaCl (molecular weight 57.5), while America typically reports sodium use (atomic weight 23). So, the 7.5 grams of salt (NaCl) that brought great health improvements to England is 7.4 *23 / 57.5 = 3 grams of sodium.
- It is difficult to draw individual conclusions without more information on salt-resistant and salt-sensitive subgroups and each subgroup's health outcomes on reduced salt intake.
Population advice vs. individual advice
England's experiment showed that if salt (sodium chloride) is restricted in processed and packaged foods, the country had fewer strokes and heart attacks, and overall blood pressure was better controlled.
However, the country is composed of many subgroups, and the health benefits may be primarily in some subgroups and not others. Suppose we don't have any information about which subgroups benefited and which did not. In that case, it is hard to give individual advice, and we may only be able to provide population advice. If we have information about subgroups that benefit or do not benefit, then we can better give individual advice.
Confounding factors can also make it difficult to determine the best advice. For example, how did England's experiment restricting sodium in processed foods improve health outcomes? 61% of the sodium salt England used was from processed foods (FDA reports in America that over 70% of sodium intake is from processed foods). Processed foods are not suitable for our health compared to whole, natural foods for many reasons. Did the reduction in salt in processed foods make them less desirable and cause the population to eat less processed foods? If so, how much of the health benefits came from less of the non-salt dangers of processed foods, and how much from less salt?
I guess the 2011 decision in England to change from forced limits on salt in processed foods to just recommendations was due to pressure from the food industry. The food industry is interested in profits and selling more processed foods. The food industry pressure on the government was likely caused by a drop in sales of processed foods, which were less tasty (or addictive) with less salt.
It makes sense for a government to restrict salt in processed foods to improve population health and lower health care costs. But it may not make sense to tell everyone to limit salt in their diet unless they are salt-sensitive. We know it does make sense to tell everyone to avoid processed food and to have a healthy diet with whole, real food.
American Heart Association guidelines
"The American Heart Association recommends no more than 2,300 mg a day and moving toward an ideal limit of no more than 1,500 mg per day for most adults." (https://www.heart.org/en/healthy-living/healthy-eating/eat-smart/sodium/how-much-sodium-should-i-eat-per-day).
They also state that "more than 70% of the sodium Americans eat comes from packaged, prepared and restaurant foods — not the salt shaker. ... Americans consume far too much sodium — about 3,500 milligrams daily."
If the above numbers are correct, a quick math calculation is that at least 2,450 mg of daily 3,500 mg of sodium Americans take are from packaged, prepared, and restaurant foods. The other 1,050 mg sodium is from whole natural foods and salt added in home cooking or at the table from salt shakers. If we take the advice of health experts to avoid processed and packaged foods (and restaurants), then we probably have a low salt intake for our cardiovascular system and blood pressure.
There is controversy over whether available evidence for the population supports keeping sodium <2,300 mg, much less 1,500 mg. A 2021 review article on the evidence concluded:
We suggest that, until new data emerge (ideally from large clinical trials), the optimal sodium intake should be in the range between 3 and 5 g/day. Most Americans (i.e., about four out of five people) have sodium intakes below 5 g/day, and in these individuals there is little evidence that lowering sodium will reduce cardiovascular events or death. Therefore, efforts to reduce sodium intake in entire populations cannot be justified. A more appropriate strategy would be to use targeted approaches directed at individuals consuming high amounts of sodium (>5 g/day), which, in the US, may also be diets with high intakes of processed foods, where the focus should be on overall health dietary patterns. At-risk individuals, especially the elderly and people with hypertension, it is reasonable to suggest avoiding excessive sodium intake (i.e., >4 g/day), in the absence of orthostatic intolerance syndromes.
Based on this, perhaps the advice focus in general should be to avoid processed foods and, when using restaurants, only order low-sodium dishes.
The 2013 report by the Institute of Medicine, Sodium Intake in Populations: Assessment of Evidence, concluded in part:
while the current literature provides some evidence for adverse health effects of low sodium intake among individuals with diabetes, CKD, or preexisting CVD, the evidence on both benefit and harm is not strong enough to indicate that these subgroups should be treated differently from the general U.S. population. Thus, the committee concluded that the evidence on direct health outcomes does not support recommendations to lower sodium intake within these subgroups to or even below 1,500 mg per day.
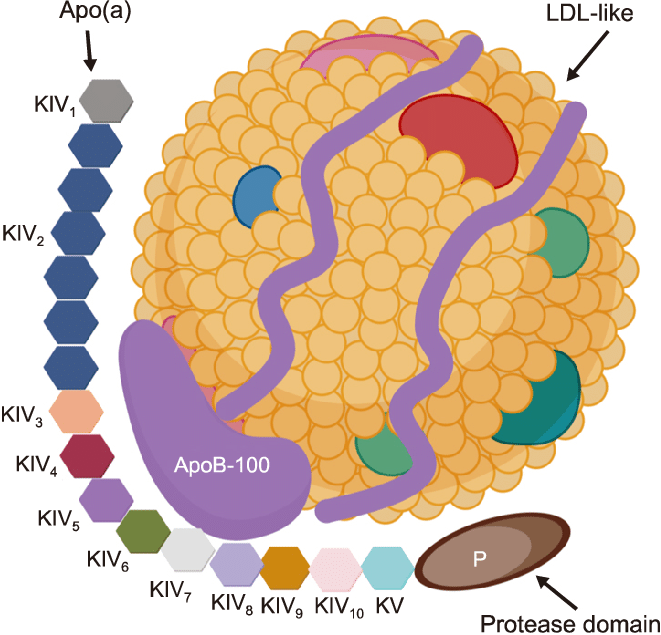
Blood pressure and salt (sodium and potassium salts)
When discussing blood pressure, salt is only one contributor. Being above ideal body weight, lack of exercise, eating ultra-processed foods, and having older kidneys that are impaired are significant contributors to increasing blood pressure. The first three and salt intake can be lifestyle modifications. We have less control over making our kidneys younger. The Yanomamo tribe appears to support the idea that a lifelong, deficient sodium diet with its resultant low blood pressure likely means the kidneys do not age as far as getting significant impairment over 50+ years.
The evidence is good that lowering sodium lowers blood pressure but less good for reducing cardiovascular events and death. This is true for the population as a whole. The population comprises millions, all of whom may differ in sodium and blood pressure interaction. More on this below under who is salt resistant. Bottom line: A lower salt intake lowers blood pressure, but in some people, it may have a minor effect and, in others, a major one.
The evidence is also strong that increased potassium intake (such as using a potassium chloride salt substitute instead of sodium chloride) significantly reduces strokes and blood pressure. The effects of sodium salt on raising blood pressure are greater when potassium intake is low (see here). As a 2013 study showed, potassium reduces blood pressure and strokes:
High quality evidence shows that increased potassium intake reduces blood pressure in people with hypertension and has no adverse effect on blood lipid concentrations, catecholamine concentrations, or renal function in adults. Higher potassium intake was associated with a 24% lower risk of stroke (moderate quality evidence). These results suggest that increased potassium intake is potentially beneficial to most people without impaired renal handling of potassium for the prevention and control of elevated blood pressure and stroke.
The World Health Organization also reports, "Increased potassium intake results in reduced blood pressure and may also result in decreased cardiovascular disease." They are preparing guidance on using low-sodium salt substitutes as a blood pressure-lowering strategy. In their statement, they say, "These alternative salts include less sodium than regular salt and often add potassium chloride with or without other agents to achieve a flavor similar to regular salt."
Kidney processing of salt and blood pressure
Blood pressure = cardiac output x total peripheral resistance.
Cardiac output increases when the blood volume expands due to taking in more water and salt.
When excess blood flows through a tissue, autoregulation constricts the vasculature to decrease the local blood flow back to normal. When cardiac output increases so that an excess amount of blood flows through all the tissues, the autoregulation causing vascular constriction is everywhere so that total peripheral resistance increases. Thus, the blood pressure goes up.
Guyton and Hall's Textbook of Medical Physiology (14th Ed, 2020, p. 233) states that a 5-10% increase in cardiac output can increase the mean arterial pressure from a normal 100 mm Hg to 150 mm Hg!
When healthy people drink lots of pure water, their kidneys excrete excess water almost as fast as it is taken in. Hence, any increase in arterial blood pressure due to the extra water increasing cardiac output is so transitory to be negligible.
However, getting rid of salt when added to water (such as in soft drinks) is not as easy. The salt increases blood osmolality, which causes the pituitary gland to secrete more antidiuretic hormone. This, in turn, causes the kidneys to reabsorb much of the water they would otherwise be excreting.
As Guyton and Hall (2020, p. 233) put it:
increasing salt intake in the absence of impaired kidney function or excessive formation of antinatriuretic hormones usually does not increase arterial pressure much because the kidneys rapidly eliminate the excess salt, and blood volume is hardly altered.
Unfortunately, impaired kidney function is not uncommon, and there are no symptoms in the early stages. A normal kidney has an eGFR>=90 and no protein in the urine. Some labs do not even report an eGFR>60 due to concerns about eGFR over 60 inaccurately measuring true GRF. In adults, impaired kidneys may be present in 10-30% or more.
Angiotensin II is a powerful controller of sodium excretion in the kidneys. It increases sodium reabsorption in the kidneys, so a decreased level of angiotensin II allows the kidneys to excrete more sodium and water. As Guyton and Hall (2020, p. 397) report in impaired kidneys that are not able to effectively decrease renin and angiotensin II formation:
Threfore, when sodium intake is raised, much greater increases in arterial pressure are needed to increase sodium excretion and maintain sodium balance. For example, in most people, a 10-fold increase in sodium intake causes only an increase of a few mm Hg in arterial pressure, whereas in subjects that cannot supress Ang II formation appropriately in respose to excess sodium, the same rise in sodium intake causes blood pressure to rise by as much as 50 mm Hg.
The suppression of angiotensin II is the mechanism used by the blood pressure medications called ACE inhibitors and ARBs (angiotensin receptor blockers). The ACEI drugs work by inhibiting angiotensin I from forming into angiotensin II, in addition to other actions such as additional vasodilatation and increased kinin levels that can cause a cough. The ARB drugs work by blocking angiotensin II from locking onto the AT1 receptors on the cell membrane, thereby inhibiting the action of angiotensin II. ARB drugs do not block the other angiotensin II receptor, AT2, which ACEI drugs indirectly do by inhibiting the formation of angiotensin II—(UpToDate, RAS inhibition in the treatment of hypertension, accessed 5/27/2024).
These medications allow the impaired kidneys to excrete salt and water at normal blood pressure by reducing angiotensin II. Without medications in a hypertensive patient, the kidneys will still excrete the salt and water they must get rid of, but they require higher blood pressure to do so.
Who is salt-resistant?
A 2024 review article noted:
For approximately one-third of otherwise healthy individuals (and >50% of those with hypertension), the effect of salt intake on blood pressure elevation is exaggerated; such people are categorized as salt sensitive and salt sensitivity of blood pressure is considered an independent risk factor for cardiovascular disease and death. The prevalence of salt sensitivity is higher in women than in men and, in both, increases with age.
The authors explain two main theories about why some are salt-sensitive and others salt-resistant. One is Guyton et al.'s kidney-focused hypothesis with impairment of angiotensin II control discussed above. The other is vascular dysfunction theory, which is about poor regulation of vascular tone in resistance arteries and arterioles. They also note that the gut microbiome could be involved, based on a variety of findings, including "Chronic angiotensin II infusion, a classic pharmacological model of salt sensitivity, decreases gut bacterial biodiversity, increasing the ratio of Firmicutes to Bacteroidetes, which are the major bacterial phyla. Disturbances in this ratio are found in many human bowel pathologies. In angiotensin II-dependent hypertension, the antibiotic minocycline rebalances the Firmicutes to Bacteroidetes ratio (of the gut microbiome), reducing BP."
As there is no specific test for who is salt-resistant, the practical way to find out is to monitor blood pressure daily and see the difference in blood pressure readings during a week of very low salt intake and then how much it increases with a high salt intake the following week. It is essential to keep potassium intake constant for the two weeks to accurately compare sodium's effect on blood pressure.
Which salt is best?
A potassium-containing salt substitute (e.g., Nu-Salt #ad) is best for home cooking or salt shaker use. Exceptions include those with significant chronic kidney disease or hyperkalemia. Always discuss the changes you plan to make with your personal physician, as this blog is for medical education, not specific medical advice for your circumstances.
Avoid processed and packaged food, which automatically removes the majority of salt from your diet. Instead, focus on eating real, whole food with minimal processing. Read the book Ultra Processed People (#ad).
If you are salt-resistant and want to use a sodium chloride-based salt, you may want to consider salt with a lower sodium content, such as Baja Gold Salt (#ad), which is only 85% sodium chloride. The rest includes other beneficial minerals, including potassium and magnesium.
#ad:(As an Amazon Associate, I earn from qualifying purchases through amazon links, at no cost to you, which helps support this blog)