Tirzepatide for Sleep Apnea 2
The SURMOUNT-OSA study showed tirzepatide (Zepbound from Eli Lilly) effectively treats sleep apnea.
The SURMOUNT-OSA study was published in the New England Journal of Medicine on 6/26/24. My prior post reviewed sleep apnea and the very effective treatment results of tirzepatide (brand name Zepbound from Eli Lilly).
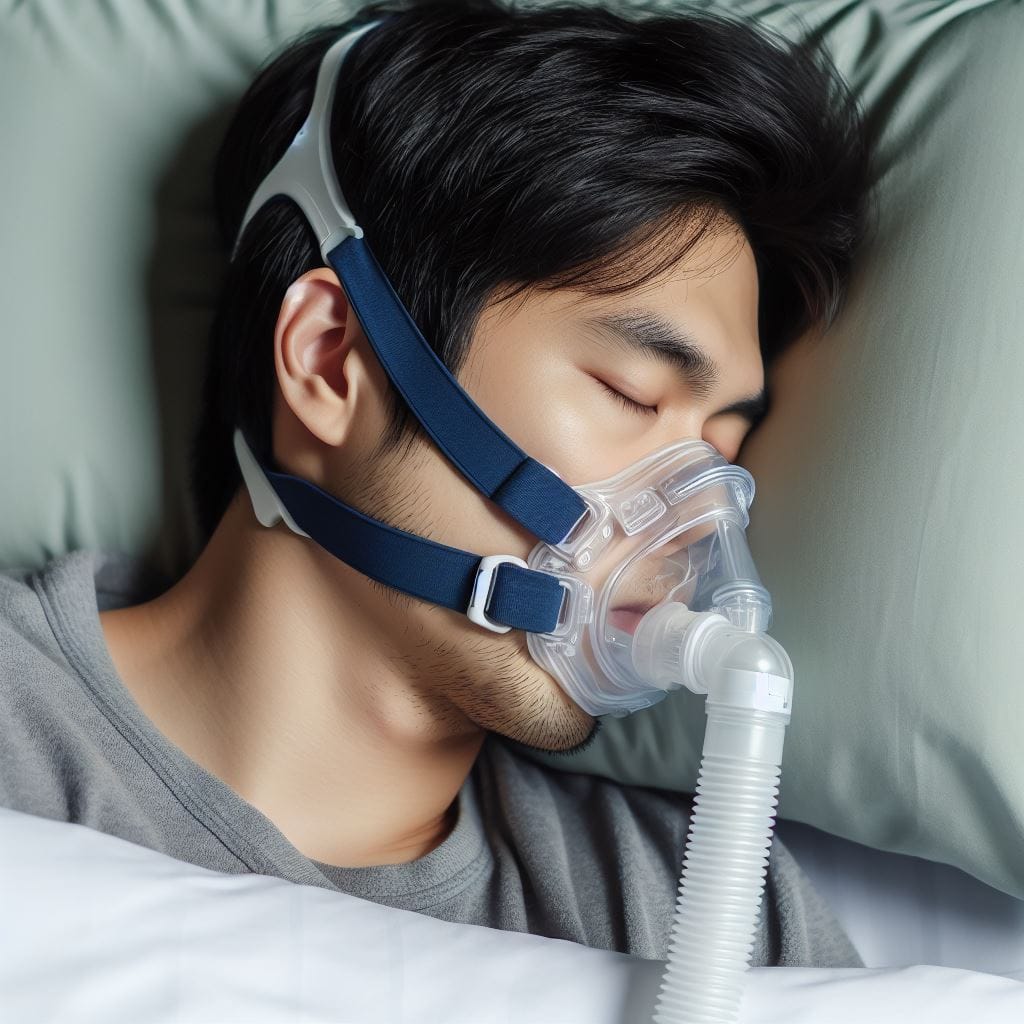
Resmed, Inc., the primary maker of CPAP machines for sleep apnea, saw its stock price drop 11% when the NEJM article was published. Lilly has applied for FDA approval for the indication of sleep apnea, and based on the trial data, it is likely that they will get it. After that, Medicare will probably cover it for the indication of sleep apnea, even though Medicare does not cover weight loss drugs such as tirzepatide for the indication of obesity. The timing may be perfect for Lilly since on Jan 1, 2025, the Inflation Reduction Act included a Medicare Part D provision that will limit out-of-pocket drug expenses to $2,000 annually (as they did for Wegovy for certain cardiovascular risks; see my blog post here).
Study Results
The study participants were all obese, so although sleep apnea occurs in people of normal weight, we don't know if tirzepatide helps sleep apnea in this group as they were not included in the study. Does tirzepatide help sleep apnea ONLY by reducing weight? The study does not answer this, but it is possible.
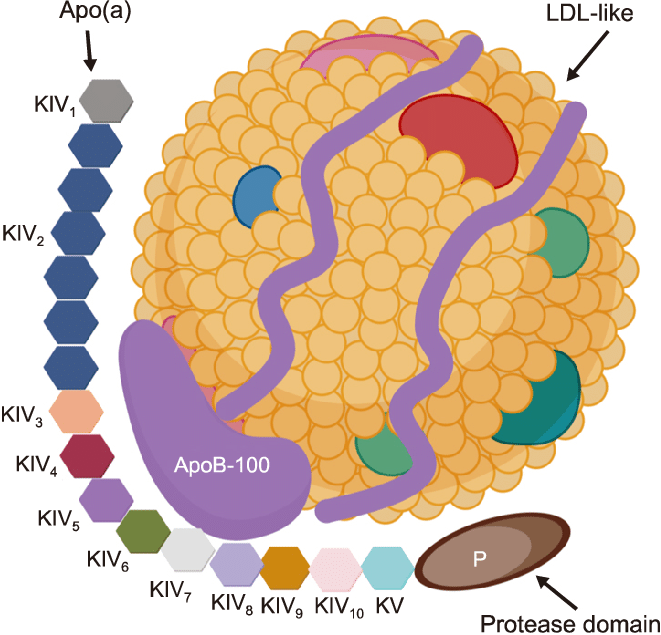
The Apnea-Hypopnea Index (AHI) is the sum of the number of apneas and hypopneas during sleep. These are measured during a sleep study. Normal is under 5 per hour. Sleep apnea is classified as mild (AHI 5-14), moderate (AHI 15-29), or severe (AHI 30 or higher). For those using CPAP (continuous positive air pressure) for at least 6 hours nightly, the AHI normalizes to less than 5 per hour.
Although some on tirzepatide may reduce their AHI enough to no longer need CPAP, the average AHI of participants at baseline was about 50. On average, AHI was reduced in the treatment groups by 27-30, so for most, CPAP would need to be continued in addition to tirzepatide.
If a sleep apnea patient continued tirzepatide indefinitely, not just for 1 year of the study duration, would more improvement happen where CPAP could be eliminated for most? The answer is unknown. The average weight loss in the treatment groups was 17-20%. The average starting weight was about 115kg (253 pounds; BMI 38-40). Depending on how much more weight was lost in the second year of treatment, perhaps more sleep apnea patients would have a low enough AHI to no longer need CPAP.
Approvals and Cost
The FDA is expected to approve tirzepatide for sleep apnea this year. Medicare may likely agree to cover its cost for sleep apnea only starting 1/1/2005 or soon thereafter.
Already, tirzepatide is a significant driver of profit for Lilly, whose website states:
Revenue in Q4 2023 increased 28%. New Products revenue grew by $2.19 billion to $2.49 billion in Q4 2023, led by Mounjaro and Zepbound.
Tirzepatide is marketed under two brand names. Mounjaro is approved for diabetes and is covered by many insurance companies only for those with diabetes. Zepbound is approved for weight loss and is generally not covered by insurance companies. A month's supply of the weekly injection is over $1,000 out of pocket unless insurance pays for it.
When non-Medicare insurance covers it for sleep apnea, which is also likely to happen, they might put it at a high-tier level where the patient has to pay half or or a substantial percent of the cost. Given the annual cost of Zepbound, which is over $12,000, this may be out of reach of most, but not all, those with private insurance.
When Medicare agrees to cover it, the patient's out-of-pocket cost for all covered drugs for a year will be capped at $2,000 starting 1/1/25 under the Inflation Reduction Act. Many are already paying co-pays that add up to hundreds or even thousands of dollars a year for the medications they are on. If a patient has sleep apnea, they will likely be able to get Zepbound for a relatively low out-of-pocket cost next year, and I suspect many will.
Numbers of Patients
"Obstructive sleep apnea affects 17% of women and 34% of men in the US and has a similar prevalence in other countries" (Gottlieb & Punjabi, 2020). It is more common in the elderly. If we conservatively estimate there are 100 million men and 100 million women adults in the US, then over 50 million have sleep apnea. Most are not yet diagnosed; many may have only a mild case. Tirzepatide is likely to be approved and covered only for moderate-severe cases of sleep apnea.
As a primary care doc retired less than a year ago, I've seen that:
- Many obese patients who likely have sleep apnea are not interested in having a sleep test to get a formal diagnosis and treatment with CPAP.
- Many non-diabetic obese patients would like to be on a drug like Zepbound to lose weight but cannot afford it, and it is not covered under their insurance.
- Many formally diagnosed sleep apnea patients have given up on their CPAP as something they cannot or do not want to tolerate.
- Therefore, I suspect that in the coming few years, sleep labs will have long waiting lists as many patients seek to formalize a sleep apnea diagnosis to have their insurance cover Zepbound so that they can lose weight.
While it is hard to predict how many millions of patients with sleep apnea will get started on Zepbound in the coming few years, at the current prices, this would cost:
- Over $12,000 per person per year
- Over 12 Billion dollars per 1 million patients per year
- Over 120 Billion dollars per 10 million patients per year
Even if there are significant discounts, cutting this in half, given Medicare's 2025 plan limiting out-of-pocket drug costs to $2,000 annually, Medicare may be spending billions more for this drug for sleep apnea. This may mean significantly higher Part D monthly drug premiums for everyone.